Post Radiation Brain Necrosis
Could be that because you are within the post-radiation window in which necrosis would be likely to be showing up. Bevacizumab is effective and safe for the treatment of RN after SRS for brain metastasis.

Coglomerate Lesions Tuberculoma Radiology Medicine Science Biology
RBN is a serious complication of intracranial and skull base tumors after radiotherapy.

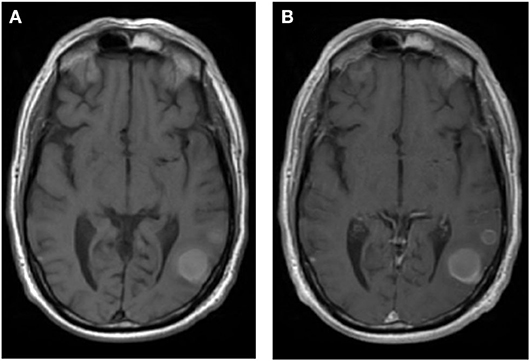
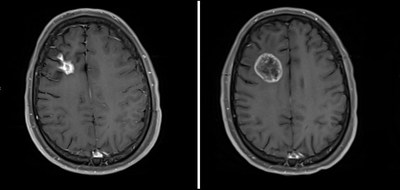
Post radiation brain necrosis. In the past due to the lack of effective treatment radiation brain necrosis was considered to be progressive and irreversible. The major complication of radiosurgery is the development of symptomatic Radiation Necrosis requiring prolonged administration of steroids and reoperation. Incidence is highest following high-dose local radiation such as stereotactic radiosurgery SRS or brachytherapy with reported rates after SRS ranging from 4-19 4-7. Radiation-induced late brain injury consisting of vascular abnormalities demyelination white matter necrosis and cognitive impairment has been described in patients subjected to cranial radiotherapy for brain tumors. The present report describes our experiences with CT EEG and neurological examination in transient adverse radiation reactions occurring 2-8 months after irradiation of the brain. One of these late effects is radiation necrosis RN.
Brain necrosis resulting from therapeutic irradiation to the whole brain partial brain or stereotactic radiosurgery SRS is commonly referred to as radionecrosis RN. This can happen 6 months to 2 years after the radiation. Failure to recognize the syndrome may also lead to recraniotomy followed by neurological sequelae. Accurate diag-nosis of these lesions greatly influences subsequent man-agement from cessation of current treatment to future. The resulting brain tissue necrosis can occur as early as 6 months after the radiation treatment. Radiation necrosis is a known complication following radiation therapy for extracranial and intracranial malignancies and should be considered in patients after radiotherapy for NPC presenting with neurologic complaints Cheng et al 2000.
Radiation injury is usually found around the tumor bed but it can occur anywhere within the irradiated field and rarely even on the contralateral side. 31 Recognition of the risk factors for radiation necrosis has resulted in a decrease in incidence. RN is an infrequent yet well recognized SRS treatment risk for malignant metastatic and certain benign tumors such as AVMs. 45 Although cases of radiation necrosis have been reported as early as 3 months and as late as 46 years 4 it usually. Previous studies included data on the frequency of RBN after irradiation of nasopharyngeal carcinoma NPC glioma brain metastases and intracranial arteriovenous malformations and are summarized in Table 1 6. In this context bevacizumab offers symptomatic relief a reduction in steroid requirement and a dramatic radiographic response.
Radiation necrosis typically occurs 12 years after radiation but latency as short as 3 months and as long as 30 years have been reported. The past year has been brutal with extreme fatigueexhaustion. Although I told my radiationoncologist about this I was given no reasons for it. After doing much research on the subject it does happen slowly the good brain cells start to die. However the lesion may also represent other pathology such as cerebral radiation necrosis RN. Then 9 months ago I started fainting now being told it was most likely seizures.
Soft-tissue radionecrosis of the brain generally occurs in the area of the brain where the tumor was radiated. Radiation-induced brain necrosis RBN is a serious complication of intracranial as well as skull base tumors after radiotherapy. Radiation-induced brain necrosis usually occurs 10 months after radiotherapy and is a late complication of radiotherapy. Bevacizumab as a treatment for radiation necrosis of brain metastases post stereotactic radiosurgery. Symptomatic RN can cause significant morbidity and should be managed pro-actively. However in my experience this disease likes to nest in necrotic clumps and while everyone is chasing around trying to fix the necrosis the cancer is secretly festering in the necrosis.
There is no single modality which can reliably distinguish RN from recurrent tumor and a multi-modal approach is often required. Bony necrosis osteoradionecrosis When blood supply to bones is restricted or cut off they can become damaged. The rate of reoperation is 30-40 usually within six months. The diagnosis of RN itself may be quite challenging as conventional imaging is frequently not able to differentiate RN from BM recurrence. Brain radiation necrosis RN represents one of the main limiting toxicities generally occurring from 6 months to several years after treatment. The brain tissue necrosis is a delayed effect of radiation therapy and can occur several years after the radiation treatment but it usually occurs within.
Radiation necrosis RN will be increasingly encountered due to the widespread use of SRS. However SRT may have some disabling side effects. Moreover in patients who are planned to undergo brain irradiation after definitive treatment for NPC the exact previous treatment. Radiation Necrosis occurs more commonly after radiosurgery but can occur after conventional Whole Brain Radiation therapy as well. The prognosis for patients with RN is typically poor with one study citing a median survival time of 30 months following the development of necrosis 3. Enhancing lesion in the brain following radiotherapy is usually related to tumor progression or recurrence.
Cerebral brain radiation necrosis Radiation to the head and neck can sometimes damage sensitive brain tissue. Symptoms and sometimes cause brain necrosis. 5 The incidence of radiation necrosis varies ranging from 1 to 30. As the survival of patients with BM is being prolonged due to improved systemic therapy ie for better extra-cranial control and increased use of SRS ie for improved intra-cranial control patients are clinically manifesting late effects of radiotherapy. Radiation soft-tissue Injury Radiation can disrupt blood supply to soft tissue causing it to break down. Her doctor said that she didnt think that Mom was even going to live this long so.
Pseudo-progression usually occurs within 2 months after treatment which is earlier than the typical period of radiation-induced brain necrosis after radiotherapy alone. Post radiation necrosis of right temporal lobe of brain. Types of Radiation Necrosis. I am 2 years 11 months post radiation for NPC.
Frontiers A Radiation Oncology Approach To Brain Metastases Neurology

Systemic Lupus Erythematosus Cns Vasculitis Radiology Case Radiopaedia Org Radiology Lupus Mri Brain

Dysembryoplastic Neuroepithelial Tumour Dnet T2 Bubbly Radiology Radiology Imaging Pediatric Radiology

Vasculary Territories Brain Brain Anatomy Mri Brain Radiology Imaging

Pin By Jojo Al On Neuro Neurological Assessment Neurology Medical Anatomy

Effect Of Bevacizumab On Radiation Necrosis Of The Brain International Journal Of Radiation Oncology Biology Physics

Cerebral Radiation Necrosis Radiology Case Radiopaedia Org Radiology Mri Brain Medical Imaging

Pin By Iskander On Mri Ct Medical Anatomy Brain Anatomy Radiology

Inflammation Flare And Radiation Necrosis Around A Stereotactic Radiotherapy Pretreated Brain Metastasis Site After Nivolumab Treatment Journal Of Thoracic Oncology
New Trial Seeks To Reverse Effects Of Dead Brain Tissue Caused By Radiation Biospace

Distinguishing True Progression From Radionecrosis After Stereotactic Radiation Therapy For Brain Metastases With Machine Learning And Radiomics International Journal Of Radiation Oncology Biology Physics
Posting Komentar untuk "Post Radiation Brain Necrosis"